A Change Is Needed
In May 2018, the New England Journal of Medicine (NEJM) published an editorial calling for a paradigm shift in the deployment of preventive interventions.
The key points are:
- Clinical studies have proven behavioural interventions, such as the Diabetes Prevention Program (DPP), to be highly effective.
- These interventions are being adopted very slowly owing to old financing models by payors and scalability challenges for providers.
- Digital interventions can overcome these barriers and enable better health at lower cost.
While the NEJM article was written from a US perspective, it is pertinent to healthcare stakeholders in Asia. Especially because payment models in Asia are diverse – healthcare costs are not borne by insurers alone, but also employers, governments and individuals. Chronic diseases like diabetes will be the key driver for rising healthcare costs in Asia over the next 10 years.
The Situation Today in Asia
Today, at least 60% of people with diabetes live in Asia, half of those in India and China. That’s more than 230 million people. And the prevalence is increasing significantly with time – in Singapore, 11.3% of the population has diabetes, a rise from 8.2% just 6 years before. This trend means that the global economic burden of diabetes is projected to almost double from 2015 to 2030.
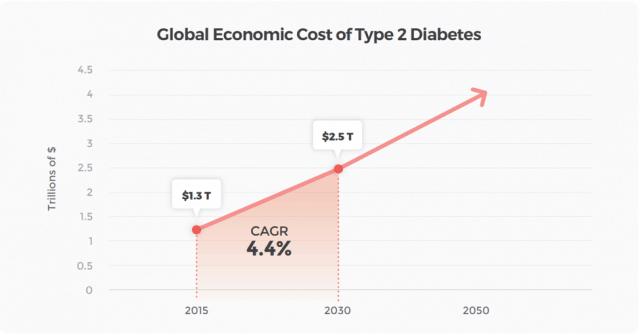
Figure 1: Global Economic Cost of Type 2 Diabetes[1]
What does this mean for organisations? In 2010, total economic costs per working-age patient in Singapore were estimated at US$5,646, of which 42% were direct medical costs and 58% indirect productivity-related losses[2].
Let’s do a back-of-the-envelope calculation: In an organisation of 1,000 people, approximately 200-300 of them could be at-risk of diabetes, or already have diabetes. This could be costing the organisation a staggering USD$1,600,000 (USD$5,646 x 300) per year in direct costs and productivity losses.
Targeted, preventive interventions are a solution. Interventions such as the Diabetes Prevention Program (DPP) have been proven to be highly effective in long-term studies. The DPP reduced the incidence of diabetes by 58% compared with placebo among people with elevated fasting glucose, over a mean follow-up of 2.8 years. While this study was conducted in the US, these results are likely applicable to the Asian population too: the Da Qing study in China showed a 42% reduction in diabetes incidence over 6 years in the lifestyle intervention group compared to a control group.
Traditional Interventions Face Many Challenges
Despite these findings, insurers, large employers and governments in Asia have been slow to adopt and provide coverage for such interventions. The question is why? There are two major issues that are barriers to more widespread adoption: .
1. Health financing models have not caught up with current needs and opportunities
Health financing models in most Asian countries favour treatment over prevention. For example, new and costly medications for cancer treatment which are not curative but may prolong life for a few months are often reimbursed when prescribed by the oncologist, with few questions asked. This drives up healthcare costs. On the other hand, preventative interventions have to meet a higher standard of cost-effectiveness within a specified time frame, before even being considered for reimbursement. From an economic standpoint, it is far more rational to reallocate expenditure towards interventions that result in improvement in the aggregate health of the population, and also cost savings.
2. Scalability issues in implementing traditional preventive interventions
Many preventive interventions were conceptualised as face-to-face intervention spanning several months. This was before the advent of smartphones. For example, the DPP is highly labour-intensive, requiring large numbers of coaches, case managers and administrative staff for delivery. As an offline intervention, its availability is limited by geography. For participants, scheduling challenges and lack of time often result in poor enrollment numbers.
Digital Therapeutics are the solution
In a nutshell, we know what needs to be done to mitigate rising healthcare costs, but traditional ways are expensive and labour-intensive. Technology however offers a radically different way to do the same thing cheaply, and at scale. In particular, digital therapeutics show great promise – not to replace health professionals but to massively increase healthcare productivity.
Digital therapeutics are digital interventions capable of delivering clinically significant outcomes such as weight loss or improved diabetes control, similar to those of prescribed drugs. They are usually developed on a foundation of science, drawing upon core elements from clinically-proven interventions. They also leverage consumer and mobile technology to deliver an experience that is accessible, simple-to-use and engaging.
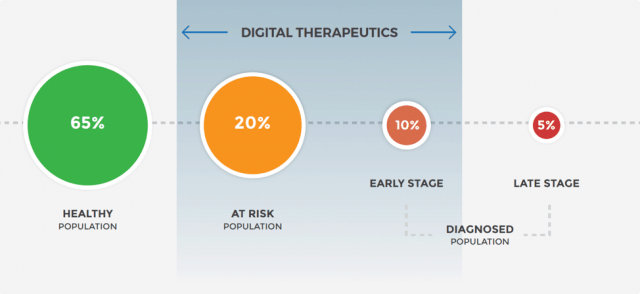
Figure 2: Population segments, in the spectrum of diabetes, where digital therapeutics fit in best
Smartphones are ubiquitous today with high penetration in developed and developing countries. Digital therapeutics are not restricted by geography and can be deployed quickly, and at scale to serve large populations. They can be packaged as an out-of-the-box solution that minimises hassle and overhead costs for HR and administrative departments. Digital therapeutics are well-suited for the at-risk (eg. prediabetes) and early-stage
In particular, digital therapeutics do the following things better and inexpensively:
A.Tracking of personal health data and Personalisation
Digital tools such as apps and wearables allow low-effort and real-time tracking of participants’ health. This data can then be used to personalise the intervention to the participant. Eg. Rise is photo-based food tracking app that connects a user with a nutrition coach. The interface allows the coach to visually understand a persons’ eating habits over time and guide accordingly.
B. Regular Engagement
The use of technology allows more frequent, less time-consuming interactions with participants around their health – a high frequency low touch model that works well for behaviour change. Eg. Pear Therapeutics has developed a digital programme for substance abuse disorders, that delivers cognitive behavioural therapy through regular lessons, self-reporting and rewards in a mobile app.
C. Social Comparison
Technology connects people, allowing them to support, motivate and encourage each other around health-related issues. This is absent in traditional healthcare delivery, where most of the interactions are between the health professional and the patient. Social elements can drive behaviour change. Eg. Leaderboards that create a sense of competition among participants, or online communities of patients who share tips and advice on how to deal with various issues that arise due to their condition.
Emerging studies are showing that online programmes result in health outcomes and weight loss similar to that seen in traditional face-to-face programmes[3]. In fact, digital therapeutics have the potential to be more effective over time, because they follow the engineering approach of build-measure-improve, resulting in shorter learning and feedback loops. Plus, the behavioural data collected can be used to personalise the intervention to the user and improve efficiencies: such as identifying participants that need more attention in a timely manner.
Importantly, digital therapeutics are an enabler of new health financing models, such as Engagement-based (payment for meaningful participation in the programme) and Outcomes-based (payment for meaningful clinical outcomes like weight loss) payments. This shares the risks between the organisation and intervention provider.
The Institute for Clinical and Economic Review (ICER), is an independent research organisation that evaluates new drugs, medical tests and other healthcare and healthcare delivery innovations. ICER published a report[4] in July 2016 encouraging payers to cover accredited DPP in a variety of formats across all plans with no copay. This includes digital programmes with human coaching, which were shown to have a net health benefit beyond usual care. The report also urges payers to establish pay-for-performance contracts with DPP providers based on participation, retention, and weight loss.
For example, Omada Health is a digital provider of diabetes prevention programs in the US. A significant part of its fee is paid out by employers only when an employee achieves weight loss during the program, which makes Omada Health accountable for the outcomes promised. This is tracked using a smart weighing scale which is sent to all participants. Omada Health is already the largest provider of DPP in the US and has reached more than 100,000 participants in the past 5 years. According to their claims analysis, employers can see $1,338 gross medical cost savings per participant over 2 years.
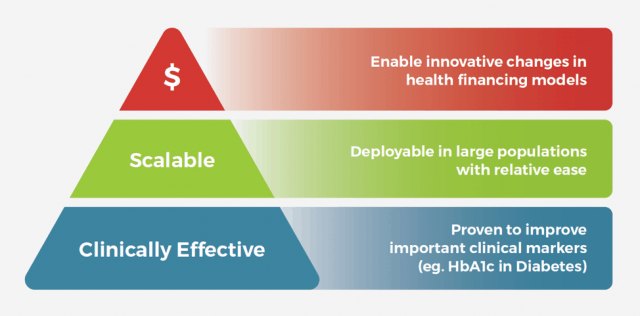
Figure 3: Three Pillars of a Successful Digital Therapeutic
The Opportunity in Asia is Huge, For Early Movers.
In Asia, there is no similar success story, yet.
For Insurers in Asia: a series of insurance innovations, such as deploying digital therapeutics, consumer engagement models, risk/pricing innovations, will create competitive advantage for early adopters among insurance firms. It is prudent to shift the focus away from short-term customer acquisition, and take a longer term perspective of their insurees’ health. Engaging insuree populations in their health with digital therapeutics have a double benefit: improving customer loyalty and thus policy renewal rates, as well as potentially reducing healthcare claims over time.
Insurers which are taking early steps in the right direction include AIA, AllLife and Oscar Health, just to name a few. AIA is a large life insurance company that offers its members AIA Vitality, an app-based wellness programme with weekly step challenges and rewards. Since its launch more than 5 years ago, it has expanded to more than 6 countries in Asia, with >100,000 users. AIA Vitality in its current form focuses mainly on fitness, an important but relatively narrow component of good health. Expanding the programme to include nutrition, mental wellbeing in the future would allow it to have an even greater impact on the health and wellness of its sizeable member population.
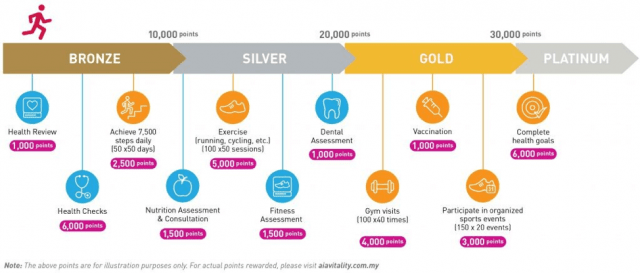
Figure 4: The AIA Vitality Journey, where you earn points for exercising and participating in various health activities. Source: aiavitality.com.my
For Employers, the benefits are direct and palpable. Besides cost savings on employee health insurance, a healthier workforce leads to better productivity and reduced absenteeism. These costs are often not directly measured today but are actually highly tangible.
And for Governments, the case is even more urgent, and stakes are higher. We have an imminent public health emergency on our hands, one that can potentially bankrupt our economic system. Successfully implementing scalable, effective preventative programmes or digital therapeutics in the community will be a vital part of a multi-prong strategy to tackle the problem.
Holmusk’s Digital Therapeutic, GlycoLeap
GlycoLeap is a digital therapeutic for people with prediabetes, diabetes and other at-risk conditions that can prevent

Figure 5: Key elements of GlycoLeap, a digital therapeutic (https://glycoleap.com)
Conclusion
In this new world of digital therapeutics, forward-thinking organisations and governments should not miss the opportunity to bravely pave the way ahead. Adopting smarter, progressive models of financing can significantly de-risk this. While healthcare claims are known to rise steadily year after year, this is not inevitable. Opportunities to bend the cost curve of healthcare must be seized, and will give visionary insurers, employers and governments a key competitive advantage in the coming future.
[1] Diabetes Care 2018 Feb; Global Economic Burden of Diabetes in Adults: Projections From 2015 to 2030
[2] BMC Public Health 2016 Feb; Current and future economic burden of diabetes among working-age adults in Asia: conservative estimates for Singapore from 2010-2050
[3] Journal of Aging and Health, Jan 2017; Outcomes of a digital health program with human coaching for diabetes risk reduction in a Medicare population.
[4] Institute for Clinical and Economic Review Jul 2016; Diabetes Prevention Programs: Effectiveness and Value
Dr. Yau Teng Yan
Dr. Yau Teng Yan is Chief Medical Officer at Holmusk, a digital health and data analytics company. Dr Yau is a practising doctor with 8 years of clinical experience in Singapore. His specialist training was in diagnostic radiology and he is an admitted fellow of the Royal College of Radiologists (London). He also did a stint in the healthcare office of the Military Medicine Institute in the Singapore Armed Forces, where he was involved in health policy decisions and health screening initiatives for servicemen. He is a big believer that technology and artificial intelligence will transform the delivery of healthcare, to achieve better outcomes, reduced costs and improved patient experience.


One comment
MiyaHealth
July 10, 2020 at 8:04 am
This is a very helpful information on digital health. Looking more from your side!!
The digital healthcare system plays a important role in reducing healthcare costs.