A step-by-step guide on how providers can make a smooth transition from fee-for-service to value-based reimbursement.
Introduction to APMs
At a time when the healthcare industry is adapting to a shift in reimbursement methodology from fee-for-service to value-based reimbursement, many hospitals find themselves in an unfamiliar position of maintaining the balance between delivering a high quality of service while reducing the total cost of care for their patients. For healthcare providers, this means integrating alternate payment models (APMs), specifically bundled payments, to improve the patient’s continuum of care.
While some critics may see this as a potential threat to their organization, initial findings point to a tremendous upside opportunity to achieve greater financial savings while increasing the quality of patient care – a classic win-win scenario for providers.
In an effort to ease hospitals into the process, the Centers for Medicare and Medicaid Services (CMS) mandated the first bundled payment model, the Comprehensive Care for Joint Replacement (CJR) model beginning October 1, 2016. The five year program applies to nearly 800 hospitals across the country with the goal of holding hospitals accountable for the entire cost of care for MS-DRG 469 and 470 (hip and knee replacements.)
Following the first year of implementation, CMS rewarded a select group of hospitals who have met (or finished below) their spend target with a bonus. Those hospitals that did not meet the spend requirements will not receive any reconciliation. After the first pilot year, providers will be held accountable by CMS in the form of a financial penalty if they’re unable to meet the target rate.
Although the first pilot year for CJR only just concluded, hospitals can expect a similar experience for other bundled payment models. Whether the bundle is voluntary or mandated, CMS or Commercial, hospitals can apply the same strategies to:
- Monitor and report trends highlighting areas of unnecessary spending
- Collaborate with physicians and other providers
Because bundled payment models represent some of the most common and high volume surgical procedures, it’s essential that your organization has developed a strategic bundled payment plan in order to meet the target rate.
Generally speaking, this 3-part engagement strategy can be applied to all bundled payment models:
- Initial assessment of your organization’s current ability to meet CMS regulations
- Action plan for implementing a bundled payment strategy
- Monitoring performance to forecast performance and revenue in bundled payment models
Step 1: Initial Assessment with Episodic Benchmark Data
Building an engagement strategy is a lot like building a skyscraper; it requires a sound foundation that can only grow when a team is committed to maintaining order within the process.
Before an organization can develop a strategy for analyzing and reporting trends in data analytics, it’s essential to gather all episodic data to perform an initial assessment on how cost-effective those services currently are. In other words, you can’t measure what you don’t know.
To get some initial bearing on where your organization stands for developing an engagement strategy, ask yourself these two questions:
- How does my organization perform today in terms of spend?
- Do I have the right team in place to lead the bundled payment initiative?
In an effort to ensure that all hospitals provide the same high quality of care for some of the most common surgeries (such as CJR), CMS assigned these spending targets based on a variety of factors.
“CJR hospitals will receive separate episode target prices for MS-DRGs 469 (Major joint replacement or reattachment of lower extremity with major complications or comorbidities) and 470 (Major joint replacement or reattachment of lower extremity without major complications or comorbidities), reflecting the differences in spending for episodes initiated by each MS-DRG. CMS will also use a simple risk stratification methodology to set different target prices for patients with hip fractures within each MS-DRG.” (CMS.gov).
“At the end of a model performance year, actual spending for the episode is compared to the Medicare target episode price for the responsible hospital.” (CMS.gov)
Understanding how your organization does perform today in meeting the CMS target rates is the best way to gauge the areas within your service line that needs the most attention for reducing unnecessary spending.
If your organization discovers that it’s already prepared to meet the spend target, ask yourself “Are there other areas within the post-acute process where we can further improve the patient’s continuum of care while cutting costs by reducing patient readmissions?” If not, begin investigating the root cause of the issue by asking “Do I have enough accurate data to highlight areas of overpayment?”
Look for factors that have the biggest influence on price reduction such as comparing utilization, readmissions, and spending to regional benchmarks. Then, you can utilize these data analytics to create an estimate for financial risks and/or opportunities.
After assessing the strengths and weaknesses in your current bundled payment plans, now is the time to evaluate your APM team to ensure that everyone knows their role and understands the impact that their role has on the entire revenue cycle.
Do I have care coordinators/nurse navigators following patients throughout the entire episode of care? Do I have a physician champion to spearhead the initiative with physicians (i.e. CMO, Lead Cardiologist, Practice Manager, etc.)?
Having the right mix of talent within your APM team is essential to putting your plan into action, but keep in mind that it requires a strong and experienced leader who understands that it may take a few rounds of trial-and-error to compile the right team.
Step 2: Action Plan
After establishing a solid foundation centered around the right personnel, you can begin implementing the engagement strategy. However, keep in mind there is a learning curve (especially for providers who were not included in the CMS pilot tests).
This action plan consists of a four-part checklist designed to provide a sustainable bundled payment plan for any organization, regardless of its size. These are the four parts:
- Design a physician engagement strategy
- Create a strategy related to the post-acute network (where applicable)
- Design a strategy for improving or maintaining quality
- Define the role of care coordinator/navigator
When developing an engagement strategy, remember to factor in the impact that other services have on your net revenue. Physicians, for example, play a large role in not only ensuring that patients receive the same high quality of care that they expect, but they also look at the entire care continuum and eliminate any procedures that could jeopardize the patients’ ability to rehabilitate properly.
Because physicians play a significant role in keeping the healthcare provider’s spending below the target rate, many organizations have reviewed gainsharing opportunities with their physician groups. For example, this incentive can be a 50-50 split of the reconciliation payment from CMS (assuming the healthcare provider finishes below the target rate) between both parties.
The next phase may involve collaborating with post-acute providers in your network to improve the quality of the patient care while cutting costs. This can only work if both parties have open lines of communication for tracking spending trends and conducting education sessions designed to teach healthcare professionals how to spot areas of excess spending.
Be aware, however, that not all providers are willing to participate (or might not be the right fit for a partnership) in these post-acute networks. Before you agree to a partnership, you should assess their willingness to partner, review their quality ratings, and assess their LOS/spending.
Lastly, an organization must appoint a care coordinator/navigator to be in charge of tracking patients and managing all bundle disclosers, waivers, and progress reports. This person will serve as the APM team leader so they’ll need to have a fully comprehensive understanding of bundled payment plans and how to lead their team day-in and day-out.
Step 3: Performance Monitoring
After your organization has developed a strategy for executing your bundled payment initiative, the final task lies in your team’s ability to track and report performance updates. In its simplest terms, performance monitoring comes down to two things:
- Providing Routine Data Analytics
- Providing Routine Calculations
Finding areas within your service line where spending can be reduced without sacrificing the quality of care is not something that your team performs once and then you’re done; it requires routine monitoring by a team that’s trained to spot certain trends in all areas of post-acute care.
When reviewing routine data analytics, your team should monitor spending and trends by patient, care setting, facility, and physician. This lets you narrow down your focus on a specific data set and prevents you from mistakenly adding data records from another point on the care path.
The same applies for reviewing routine calculations. These calculations should measure your organization’s overall financial performance as well as gainsharing estimates to provide a comprehensive cost analysis.
Prepare Now for Bundled Payment Success
At the end of the day, the shift from fee-for-service to value-based reimbursement comes down to one thing: planning ahead.
Although no team can manage their engagement strategy error free, it’s important for the APM team to be informed and address these variances before it negatively affects your reimbursement.
Healthcare providers that followed this three-part engagement strategy proved to be top performers, finishing in the top 10 percent of all hospitals in the CJR program.
In the first year of the program, these healthcare providers averaged a total reconciliation payment of $178,000 (81% higher than the average participating hospital – see Figure 1 below) or $1,445 per episode (21% higher than the average participating hospital – see Figure 2 below).
It’s also worth noting that only 382 out of about 800 hospitals required to participate (less than 50%) actually received a reconciliation payment from CMS.
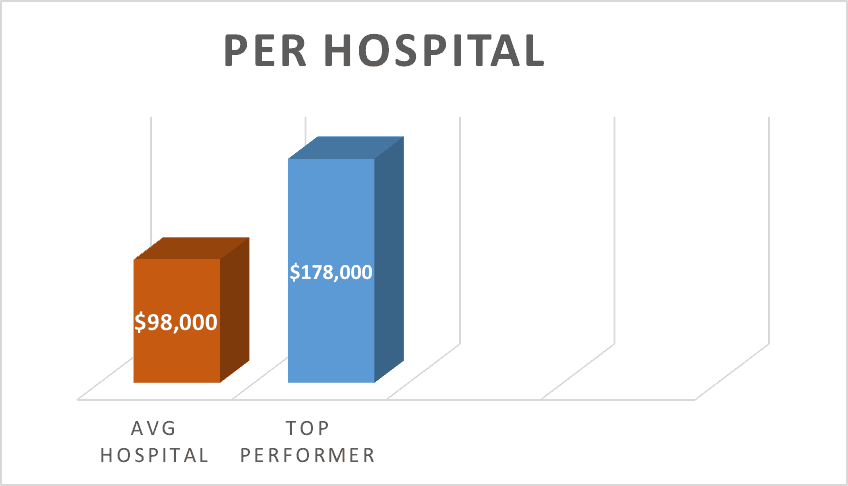
Fig.1
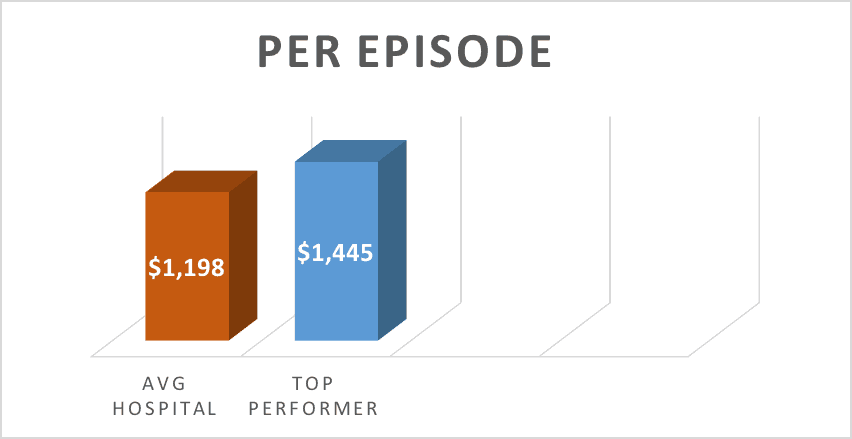
Fig.2
Again, the key to collecting maximum reimbursement within bundled payment plans is taking the time to prepare a thorough engagement strategy for your organization. This planning requires extensive research into trends and data analytics so take advantage of the opportunity to plan ahead and get your feet wet before they become mandatory and more wide-spread.
Simply put, if a provider has concerns about their ability to meet the CMS target rates, follow the steps outlined above and ensure that your APM team stays current with CMS’s updates, giving the APM team time to adjust their current engagement strategy.
Brad Josephson
Brad Josephson is the Director of Marketing at PMMC, a leading provider of healthcare revenue cycle management and contact management services utilized in hospitals and physicians offices. Brad has years of experience working with the healthcare revenue cycle and an extensive knowledge of bundled payment programs for hospitals and healthcare organizations.


